Person-centred care (PCC) is increasingly recognized as crucial for individuals living with dementia, particularly within community-based programs. As dementia rates rise globally, affecting millions and placing significant burdens on healthcare systems, the need for effective implementation of PCC in home, community, and outpatient settings becomes ever more critical. While the concept of PCC is widely advocated, practical implementation, especially in resource-constrained community programs, remains a significant challenge. This article, drawing upon a comprehensive review of existing research, identifies key tools and strategies for effectively implementing person-centred care and support (PCCS) within community dementia programs, aiming to enhance care quality and outcomes for individuals and their caregivers.
Understanding Person-Centred Care in the Context of Community Programs
Person-centred care moves beyond a disease-focused approach to prioritize the individual’s unique needs, preferences, and life circumstances. In dementia care, this means recognizing the personhood of individuals living with dementia, respecting their dignity, promoting autonomy, and fostering partnerships in care planning and delivery. Community programs, which include home care, outpatient services, and day centers, are vital in providing ongoing support for individuals living with dementia and their families. However, these settings often face unique barriers to PCC implementation, such as time constraints, limited resources, and fragmented care coordination.
The original research paper, upon which this article is based, conducted a scoping review of 22 studies to understand how to implement PCCS for dementia in community settings. The review utilized the McCormack person-centred care framework, which encompasses six key domains: fostering a healing relationship, exchanging information, addressing emotions, managing uncertainty, sharing decisions, and enabling self-management. This framework serves as a valuable tool itself, offering a structured approach to conceptualizing and implementing PCC.
Key Tools and Strategies for PCCS Implementation
Based on the synthesis of research, several key tools and strategies emerge for implementing PCCS in community programs. These can be categorized into tools for healthcare professionals, tools for individuals with dementia and their caregivers, and organizational tools.
1. Educational and Training Programs for Healthcare Professionals
One of the most consistently highlighted tools for PCCS implementation is education and training for healthcare professionals. The reviewed studies emphasized the effectiveness of in-person interdisciplinary educational meetings in improving healthcare workers’ knowledge, attitudes, and skills related to person-centred dementia care.
-
Content of Educational Programs: Effective programs should cover:
- Principles of Person-Centred Care: Defining PCC, its benefits, and ethical considerations in dementia care.
- Understanding Dementia: Brain changes, symptom presentation (including behavioral and psychological symptoms), and disease progression.
- Communication and Interpersonal Skills: Techniques for effective communication with individuals with dementia and their caregivers, including active listening, empathy, and non-verbal communication cues.
- Psychosocial Aspects of Dementia: Addressing emotional needs, managing uncertainty, and supporting personhood.
- Available Community Resources and Support Services: Familiarizing professionals with local resources to facilitate referrals and holistic care.
- Practical Application and Case Studies: Using real-life scenarios and case studies to enhance practical application of PCC principles and communication techniques.
-
Format and Delivery:
- Interdisciplinary Approach: Involving various professionals (nurses, physicians, therapists, social workers, care managers) to foster team collaboration and shared understanding.
- Interactive and Didactic Methods: Combining lectures with group discussions, role-playing, case study analysis, and video vignettes to cater to different learning styles and promote engagement.
- Ongoing Support and Mentorship: Providing continuous learning opportunities and mentorship programs to reinforce learned skills and address real-world challenges.
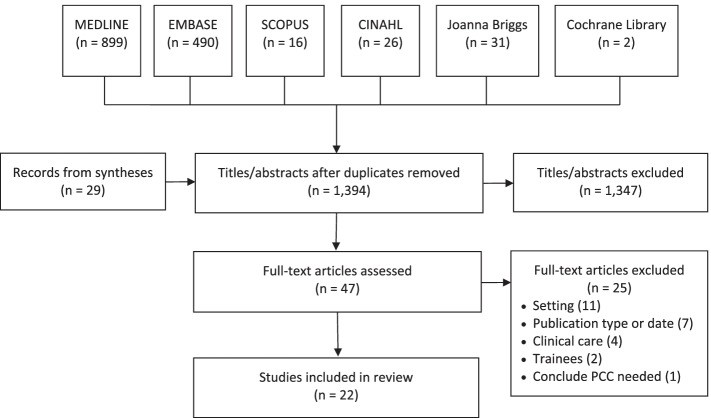 Fig. 1
Fig. 1
Alt text: PRISMA diagram illustrating the study selection process for the scoping review on person-centred care and support for dementia, highlighting the number of records identified, screened, and included.
2. Framework for Person-Centred Care and Support for Dementia
The research itself culminates in a Framework of Person-Centred Care and Support for Dementia, which serves as a practical tool for guiding care delivery. This framework, adapted from McCormack’s PCC framework, specifies key elements within each of the six domains, tailored to the dementia context.
-
Foster a Healing Relationship:
- Tools: Communication protocols that emphasize partnership, respect, and dignity. Training on building rapport and trust.
- Elements: Discuss roles and responsibilities, communicate with honesty and openness, foster trust, express caring and empathy, build rapport, ensure dignity and respect.
-
Exchange Information:
- Tools: Standardized assessment tools to explore individual needs and preferences. Communication aids for individuals with communication difficulties. Information resources for caregivers.
- Elements: Explore needs and preferences, all parties share information, provide/refer to additional information, assess and facilitate understanding, recognize the person’s life and current abilities through discussion and cues, allow time for questions.
-
Address Emotions:
- Tools: Screening tools for anxiety and depression. Training on emotional validation and empathetic communication. Access to psychosocial support services.
- Elements: Explore and identify emotions, assess anxiety or depression, validate emotions, express empathy or reassurance, provide help to deal with emotions, reframe dementia diagnosis to lessen impact, address psychosocial issues.
-
Manage Uncertainty:
- Tools: Structured routines and care plans to provide stability. Continuity of care providers to build trust and understanding. Advance care planning resources.
- Elements: Raise and discuss uncertainties, explore and assess uncertainties held by affected persons, use problem-focused and emotion-focused management strategies, create stability through routines and continuity.
-
Share Decisions:
- Tools: Decision aids to facilitate shared decision-making. Family meetings to involve caregivers in care planning. Advocacy services to support individuals’ autonomy.
- Elements: Raise and discuss care/support options, discuss decision process and needs, prepare persons/carers for deliberation, jointly make and implement decisions, assess decision quality, tailor care and support, mitigate family conflict.
-
Enable Self-Management:
- Tools: Activity programs promoting independence and meaningful engagement. Caregiver support groups and respite care. Information on assistive devices and home modifications.
- Elements: Describe follow-up process, provide information and training on self-care, share guidance on prioritizing self-care, offer practical advice and support for self-care, assess skills and progress, optimize independence, engage persons in meaningful activity, support carers, provide information on community support services.
This framework serves as a checklist and a guide for community programs to assess and enhance their person-centredness. By systematically addressing each domain and its elements, programs can move towards more holistic and individualized care.
3. Personalized and Meaningful Activity Programs
Engaging individuals with dementia in meaningful activities is a core component of PCCS. Personalized activity programs, tailored to individual interests, abilities, and preferences, can significantly improve mood, social engagement, and overall well-being.
- Tools:
- Personalized Music Programs: Utilizing music playlists based on individual preferences to evoke positive emotions and memories, as demonstrated in one of the reviewed studies.
- Social Visit Programs: Facilitating social interaction and engagement through structured visits from trained volunteers or students, offering intellectual and social stimulation beyond family interactions.
- Reminiscence Therapy: Utilizing life story work, photo albums, and memory prompts to engage individuals in recalling positive memories and strengthening identity.
- Adapted Activities: Modifying activities to match current cognitive and physical abilities, ensuring success and enjoyment.
These programs require careful assessment of individual preferences and abilities, and ongoing adaptation to ensure continued engagement and benefit.
4. Carer Support and Education Programs
Caregivers are integral partners in PCCS, and their well-being directly impacts the quality of care for individuals with dementia. Providing support and education for caregivers is therefore a crucial tool for PCCS implementation.
- Tools:
- Online Educational Modules: Offering flexible and accessible online resources to enhance caregiver knowledge about dementia, person-centred approaches, and stress management techniques, as highlighted by one study.
- Caregiver Support Groups: Creating peer support networks where caregivers can share experiences, receive emotional support, and learn coping strategies.
- Respite Care Services: Providing temporary relief for caregivers to prevent burnout and maintain their own health and well-being.
- Skills Training for Caregivers: Workshops and training sessions on communication skills, behavior management techniques, and self-care strategies tailored for dementia caregiving.
Supporting caregivers not only improves their well-being but also empowers them to implement person-centred care approaches within the home environment.
5. Organizational Policies and Culture Shift
Implementing PCCS requires a fundamental shift in organizational culture and policies. Tools at the organizational level are essential to create an environment that supports and promotes person-centred practices.
- Tools:
- PCC Policy Integration: Developing and implementing organizational policies that explicitly promote person-centred care principles and values.
- Leadership Support and Modeling: Leadership actively championing and modeling person-centred care, fostering a culture of respect, empathy, and partnership.
- Resource Allocation: Adequate staffing levels, time allocation for person-centred interactions, and access to necessary resources to support PCC implementation.
- Regular Audits and Feedback Mechanisms: Implementing systems to monitor the person-centredness of care delivery and gather feedback from individuals with dementia, caregivers, and staff to drive continuous improvement.
- Champions and Opinion Leaders: Identifying and supporting individuals within the organization who can act as champions for PCCS, promoting its adoption and implementation among colleagues.
These organizational tools create the necessary infrastructure and support system for healthcare professionals to effectively deliver person-centred care in community programs.
Addressing Barriers to Implementation
Despite the availability of these tools, several barriers can hinder PCCS implementation in community programs. These barriers, identified in the reviewed research, operate at different levels:
- Patient/Caregiver Level: Family conflict, caregiver reluctance to seek help, geographical or social distance between family members, and the individual’s own reluctance to engage.
- Healthcare Professional Level: Lack of knowledge and understanding of PCC, negative attitudes towards dementia, time constraints, perceived lack of control, and feeling undervalued within the organization.
- Organizational Level: Resource constraints, inadequate staffing, and a pressurized work environment.
Addressing these barriers requires a multi-faceted approach. Educational tools can address knowledge gaps and negative attitudes among professionals. Organizational tools, such as policy changes and resource allocation, are crucial to create a supportive environment. Furthermore, community programs need to actively engage with families to build trust and address their specific needs and challenges.
The Importance of EEAT and Helpful Content in PCCS Tools
For tools aimed at implementing PCCS to be truly effective and adopted, they must embody the principles of EEAT (Expertise, Experience, Authoritativeness, Trustworthiness) and be genuinely helpful to users. Educational materials should be developed by experts in dementia care and PCC. Training programs should incorporate experiential learning and real-world examples. Organizational policies should be grounded in evidence-based practices and demonstrate a commitment to ethical and person-centred values. Tools should be designed with the end-users in mind – being practical, accessible, and directly addressing their needs and challenges.
Conclusion: Moving Forward with PCCS Implementation
Implementing person-centred care in community programs for dementia is not merely an aspirational goal but a practical imperative to improve the lives of millions affected by this condition. This review underscores the availability of various tools and strategies, ranging from educational programs and frameworks to personalized activities and organizational changes. The Framework of Person-Centred Care and Support for Dementia itself serves as a valuable tool, providing a structured roadmap for programs to enhance their person-centredness.
Further research is crucial to refine these tools, evaluate their impact in diverse community settings, and develop new strategies to overcome persistent barriers. Future efforts should also prioritize understanding and addressing the specific needs of women, who are disproportionately affected by dementia both as individuals living with the condition and as caregivers. By embracing a commitment to ongoing learning, adaptation, and collaboration, community programs can effectively leverage these tools to deliver truly person-centred care and support, making a tangible difference in the lives of those living with dementia and their families.
Alt text: Framework of Person-Centred Care and Support for Dementia table, outlining the domains of the McCormack person-centered care framework and elaborated elements specific to dementia care identified in the scoping review.

