Introduction
In the demanding and critical field of healthcare, nurses stand as pillars of strength and compassion, delivering essential care to patients in diverse settings. However, the very nature of their profession, characterized by long hours, emotional strain, and constant exposure to stressful situations, places nurses at significant risk of burnout, compassion fatigue, and mental health challenges. Recognizing and addressing the well-being of nurses is not merely a matter of personal concern; it is fundamentally linked to the quality of patient care and the overall effectiveness of healthcare systems. Self-care, defined by the World Health Organization as the ability of individuals to promote and maintain their own health, becomes paramount for these healthcare professionals. To effectively engage in self-care, nurses need to first understand their own needs and stress levels. This is where the Self Care Assessment Tool For Nurses emerges as an indispensable resource.
The concept of self-care for healthcare professionals, including nurses and midwives, has gained considerable attention in recent years, moving from a peripheral consideration to a central tenet of professional practice. This shift acknowledges that nurses who prioritize their own health and well-being are better equipped to provide optimal care to their patients. As highlighted in numerous studies, the ability to engage in effective self-care is not an innate trait but a learned skill, requiring awareness, intention, and consistent practice. For nurses, self-care encompasses a broad spectrum of activities aimed at nurturing their physical, psychological, social, spiritual, and emotional dimensions.
The urgency of self-care for nurses has been further amplified by global events such as the COVID-19 pandemic, which placed unprecedented demands on healthcare systems and frontline workers. The pandemic not only intensified existing stressors but also introduced new challenges, including heightened risk of infection, increased patient loads, ethical dilemmas, and emotional exhaustion. In this context, the self care assessment tool for nurses becomes more critical than ever, serving as a proactive measure to identify nurses at risk and guide them towards appropriate self-care strategies and interventions.
This article delves into the crucial role of self care assessment tools for nurses. It explores the underlying concepts of self-care, the necessity of assessment in promoting nurse well-being, and the types of tools available or adaptable for this purpose. By understanding the value and application of these tools, healthcare organizations and individual nurses can take proactive steps towards fostering a healthier and more sustainable work environment, ultimately benefiting both caregivers and patients.
Understanding Self-Care and Its Relevance to Nurses
Self-care, in the context of nursing, extends beyond generic wellness advice; it is a tailored approach to maintaining and enhancing a nurse’s capacity to function effectively and compassionately in their demanding role. Drawing from the foundational work of Dorothea E. Orem, self-care can be viewed as actions taken to overcome limitations and maintain well-being, not just for patients, but for the caregivers themselves. For nurses, self-care is not a luxury but a professional imperative, directly impacting their ability to deliver quality care and sustain their own health over time.
The concept of self-care for nurses is intrinsically linked to several key constructs identified in the literature: mindfulness, compassion, and resilience.
Mindfulness, in this context, refers to the practice of present moment awareness, allowing nurses to recognize and manage their emotional and mental states without judgment. It involves paying attention to thoughts and feelings as they arise, enabling a more balanced and flexible response to stressful situations. Self-awareness, a closely related concept, is about understanding one’s own reactions and triggers, which is crucial for proactive self-care.
Compassion, particularly self-compassion, is another vital component. Self-compassion involves extending kindness and understanding towards oneself, especially during times of difficulty or perceived inadequacy. It is composed of self-kindness, a sense of common humanity, and mindfulness. Cultivating self-compassion helps nurses to manage the emotional demands of their work, reducing self-criticism and fostering a more supportive inner dialogue. Furthermore, understanding compassion satisfaction – the positive feelings derived from caregiving – is important for maintaining a healthy professional quality of life.
Resilience is the ability to withstand and recover from stressful events and changes. For nurses, resilience is not about avoiding stress but about developing effective coping mechanisms and the capacity for personal growth through challenging experiences. Resilience strategies include fostering social connections, promoting positivity, leveraging strengths, nurturing growth, and practicing self-care itself. Self-efficacy, the belief in one’s ability to succeed in specific tasks, is a key aspect of resilience, enabling nurses to confidently navigate workplace demands.
The absence of adequate self-care can lead to detrimental consequences for nurses, including burnout, compassion fatigue, and secondary traumatic stress. Burnout is characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment. Compassion fatigue, a more acute syndrome, combines secondary traumatic stress and burnout due to the constant demands of caring for suffering individuals. These conditions not only impact the nurse’s well-being but also negatively affect patient care, job satisfaction, and overall healthcare system performance.
Therefore, implementing self care assessment tools for nurses is a proactive approach to mitigate these risks. These tools can provide valuable insights into a nurse’s current state of well-being across these key constructs, facilitating early intervention and personalized self-care strategies.
The Necessity of Self Care Assessment Tools for Nurses
While the importance of self-care for nurses is increasingly recognized, translating this understanding into practical action requires effective assessment. A self care assessment tool for nurses serves as a structured and systematic method for nurses and healthcare organizations to evaluate an individual nurse’s self-care practices, needs, and potential vulnerabilities. The necessity of these tools stems from several critical factors:
Early Identification of Risk: Assessment tools can help identify nurses who are at risk of burnout, compassion fatigue, or other mental health challenges before these conditions become severe. By proactively measuring indicators of stress, resilience, mindfulness, and self-compassion, organizations can intervene early, providing targeted support and resources to prevent negative outcomes.
Personalized Self-Care Strategies: Self-care is not a one-size-fits-all concept. Individual nurses have unique needs and preferences. Assessment tools can provide personalized insights into a nurse’s specific areas of strength and weakness in self-care. This allows for the development of tailored self-care plans that are more effective and sustainable, addressing the individual’s specific needs and circumstances.
Monitoring Progress and Evaluating Interventions: Implementing self-care initiatives or interventions within healthcare organizations requires a way to measure their effectiveness. Self care assessment tools for nurses can be used to track changes in nurses’ well-being over time. By conducting assessments before and after interventions, organizations can evaluate the impact of programs, identify areas for improvement, and demonstrate the value of investing in nurse well-being.
Promoting Self-Awareness: The act of completing a self-care assessment tool can itself be a valuable self-reflection exercise for nurses. It encourages them to consciously consider their own well-being, prompting self-awareness about their stress levels, coping mechanisms, and self-care practices. This heightened self-awareness is the first step towards taking proactive responsibility for one’s own health and well-being.
Creating a Culture of Well-being: The use of self care assessment tools for nurses sends a powerful message within healthcare organizations: nurse well-being is valued and prioritized. It signals a commitment to creating a supportive work environment where self-care is not just encouraged but actively facilitated. This can contribute to a more positive workplace culture, improved staff morale, and reduced turnover rates.
Data-Driven Decision Making: Aggregated data from self-care assessments can provide valuable insights for healthcare leadership. It can highlight systemic stressors within the organization, identify common areas of need among nursing staff, and inform the development of organization-wide well-being initiatives. This data-driven approach ensures that resources are allocated effectively to address the most pressing needs of the nursing workforce.
Figure 1.
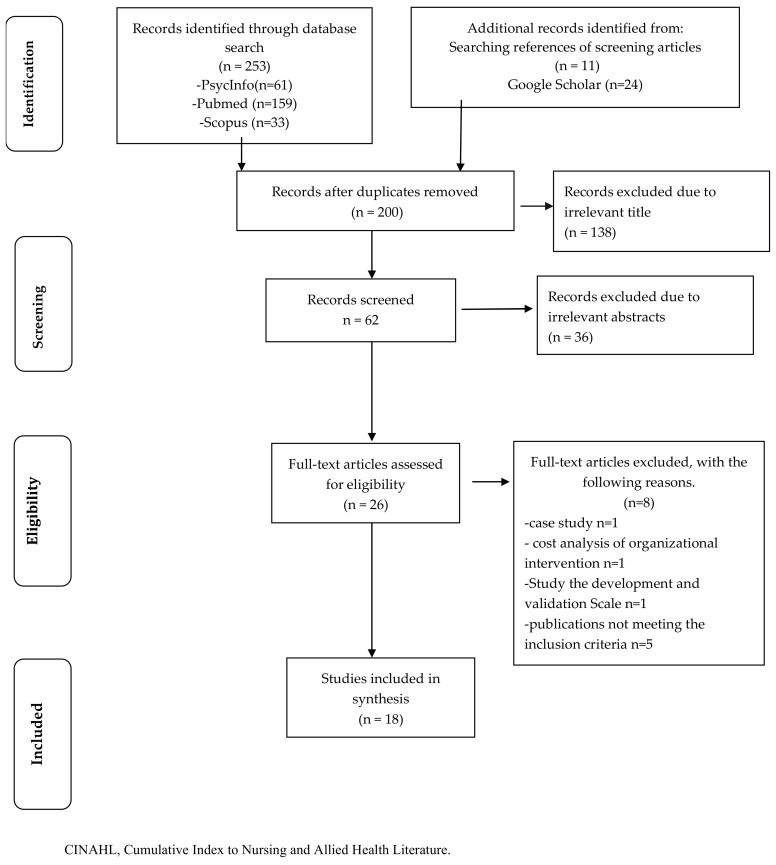 Flow chart illustrating the selection process of scoping review
Flow chart illustrating the selection process of scoping review
Figure 1: A visual representation of a systematic review process, highlighting the stages of article selection and screening, relevant to understanding how evidence on self-care assessment tools is gathered and analyzed.
In essence, self care assessment tools for nurses are not merely checklists or questionnaires; they are strategic instruments that empower nurses and organizations to proactively address well-being, foster a culture of care, and ultimately enhance the quality and sustainability of nursing practice.
Types of Self Care Assessment Tools for Nurses
While a universally standardized “self care assessment tool for nurses” might not exist, a variety of tools and approaches can be adapted and utilized to effectively assess different facets of nurse well-being and self-care practices. These tools can be broadly categorized based on the dimensions of self-care they primarily address and the methodologies they employ:
1. Burnout and Compassion Fatigue Assessments:
These tools directly measure the key negative outcomes associated with inadequate self-care in nursing.
- Maslach Burnout Inventory (MBI): A widely recognized tool that assesses burnout across three dimensions: emotional exhaustion, depersonalization, and personal accomplishment. It is frequently used in studies examining burnout in nurses and can be adapted for self-assessment or organizational surveys.
- Professional Quality of Life Scale (ProQOL): This tool measures both the positive and negative aspects of professional quality of life, including compassion satisfaction, burnout, and secondary traumatic stress. It is particularly relevant for nurses who are exposed to trauma or high levels of patient suffering.
- Compassion Fatigue Short Scale (CFSS): A briefer measure specifically focused on compassion fatigue and secondary traumatic stress, suitable for quick assessments and monitoring changes over time.
2. Resilience and Coping Mechanism Assessments:
These tools evaluate a nurse’s capacity to withstand stress and effectively manage challenging situations.
- Connor-Davidson Resilience Scale (CD-RISC): A widely used scale that measures resilience as the ability to bounce back from adversity. It assesses various facets of resilience, including tenacity, optimism, and coping skills.
- Brief Resilience Scale (BRS): A shorter, more concise measure of resilience, suitable for repeated assessments or when time is limited.
- Coping Self-Efficacy Scale (CSES): This tool assesses an individual’s belief in their ability to effectively use coping strategies in stressful situations. It can highlight areas where a nurse may need to develop stronger coping skills.
3. Mindfulness and Self-Compassion Assessments:
These tools measure a nurse’s capacity for present moment awareness and self-kindness, key components of self-care.
- Freiburg Mindfulness Inventory (FMI): Assesses mindfulness as a state of present moment awareness and acceptance, reflecting the ability to be non-judgmentally present with one’s experiences.
- Mindful Attention Awareness Scale (MAAS): Measures trait mindfulness, reflecting the frequency of everyday mindful experiences.
- Self-Compassion Scale (SCS): Evaluates self-compassion across dimensions of self-kindness, common humanity, and mindfulness, providing insights into a nurse’s capacity for self-support and understanding.
4. General Well-being and Mental Health Assessments:
These broader tools provide an overview of a nurse’s overall psychological well-being and can identify potential mental health concerns.
- General Health Questionnaire (GHQ-12): A brief screening tool for detecting general mental health distress, suitable for identifying nurses who may benefit from further evaluation or support.
- Depression Anxiety Stress Scales (DASS): Measures the severity of depression, anxiety, and stress symptoms, providing a more detailed assessment of emotional well-being.
- Ryff’s Psychological Well-Being questionnaire: A more comprehensive tool assessing multiple dimensions of psychological well-being, such as autonomy, purpose in life, and personal growth.
5. Organizational and Workplace Environment Assessments:
These tools evaluate factors within the work environment that impact nurse well-being and self-care.
- Areas of Worklife Survey (AWS): Assesses six key areas of work-life balance: workload, control, reward, community, fairness, and values. It can identify organizational stressors that contribute to nurse burnout.
- Nursing Worklife Survey (NWS): Specifically designed for nursing settings, this tool measures aspects of the work environment that influence nurse job satisfaction and well-being, such as autonomy, workload, and support from colleagues and management.
- Custom-designed organizational climate surveys: Organizations can develop their own surveys to assess specific aspects of the workplace culture related to self-care support, stress management resources, and leadership attitudes towards nurse well-being.
Table 1.
| Intervention Type | Outcome Measured | Assessment Tool Examples |
|---|---|---|
| Caring for the Caregivers (CCG) | Burnout, Stress, Well-being | Maslach Burnout Inventory (MBI), Perceived Stress Scale (PSS), General Health Questionnaire (GHQ) |
| PERMA model | Psychological Well-being | Ryff’s Psychological Well-Being questionnaire |
| Mind-body practices (Yoga) | Self-care, Burnout | Health Promoting Lifestyle Profile II (HPLP II), Maslach Burnout Inventory (MBI) |
| Mindful Self-Compassion (MSC) Training | Compassion Satisfaction, Self-compassion, Mindfulness, Burnout, Secondary Trauma | Professional Quality of Life Scale (ProQoL5), Neff Self-Compassion Scale, Freiburg Mindfulness Inventory |
| Mindfulness Based Stress Reduction (MBSR) | Compassion, Stress, Mental Health | Compassion Scale (CS), Perceived Stress Scale (PSS), Depression Anxiety Stress Scales (DASS) |
| Organizational Intervention | Burnout, Compassion Fatigue | Maslach Burnout Inventory (MBI), Professional Quality of Life Scale (ProQoL5) |
Table 1: Examples of self-care intervention types and associated assessment tools used to measure their impact on nurse well-being.
When selecting a self care assessment tool for nurses, it is crucial to consider the tool’s validity, reliability, ease of administration, and relevance to the specific context and objectives of the assessment. Often, a combination of tools addressing different dimensions of self-care may provide the most comprehensive and actionable insights.
Implementing Self Care Assessment Tools in Nursing Practice
The effective implementation of self care assessment tools for nurses requires a thoughtful and strategic approach, going beyond simply administering questionnaires. To maximize the benefits of these tools, healthcare organizations should consider the following key steps:
1. Purposeful Selection and Adaptation:
- Define Objectives: Clearly articulate the goals of implementing self-care assessments. Is it for individual nurse self-awareness, organizational needs assessment, program evaluation, or a combination?
- Choose Appropriate Tools: Select tools that align with the defined objectives and the specific context of the nursing environment. Consider factors like tool length, ease of use, cultural sensitivity, and the dimensions of self-care being assessed. Adapt existing tools if necessary to better fit the nursing context.
- Consider a Multi-Tool Approach: A single tool may not capture the complexity of nurse well-being. Consider using a combination of tools to assess different aspects of self-care (e.g., burnout, resilience, mindfulness).
2. Ensuring Confidentiality and Trust:
- Guarantee Anonymity: If assessments are used for organizational data collection, ensure anonymity to encourage honest responses. Clearly communicate how data will be used and protected.
- Focus on Support, Not Evaluation: Frame the assessment process as a supportive initiative to enhance nurse well-being, not as a performance evaluation tool. Emphasize that results will be used to guide support and resource allocation, not for individual performance reviews.
- Build Trust through Transparency: Communicate openly about the purpose of the assessments, how data will be used, and the steps the organization will take to address identified needs.
3. Integration into Workflow and Resources:
- Make Assessments Accessible: Provide easy access to assessment tools, whether online or in paper format. Consider integrating them into existing platforms or systems used by nurses.
- Offer Protected Time: Recognize that completing assessments requires time. Provide nurses with protected time during work hours to complete assessments, demonstrating organizational support for the process.
- Link Assessments to Resources: Crucially, assessments should not be a standalone activity. Establish clear pathways to self-care resources and interventions based on assessment results. This may include counseling services, mindfulness programs, stress management workshops, peer support groups, or access to employee assistance programs (EAPs).
4. Training and Support for Nurses and Leaders:
- Educate Nurses on Self-Care: Provide training and education to nurses on the importance of self-care, the concepts being assessed (mindfulness, resilience, etc.), and the available self-care resources.
- Train Leaders on Interpretation and Response: Equip nurse leaders and managers with the knowledge to understand assessment results at an aggregate level (if applicable) and to respond effectively to identified needs. Train them to promote a culture of self-care within their teams.
- Provide Ongoing Support: Self-care is an ongoing process. Offer continuous support and resources to nurses, reinforcing the organization’s commitment to their well-being. Regularly revisit assessment results and adapt strategies as needed.
5. Data Utilization for Continuous Improvement:
- Aggregate Data Analysis: Analyze aggregated assessment data to identify trends, common stressors, and areas where organizational support can be strengthened.
- Inform Program Development: Use assessment data to guide the development and refinement of self-care programs and well-being initiatives tailored to the specific needs of the nursing staff.
- Regularly Evaluate and Adapt: Periodically review the effectiveness of the assessment process and the associated self-care initiatives. Use data to make adjustments and ensure ongoing relevance and impact.
By implementing self care assessment tools for nurses in a thoughtful and comprehensive manner, healthcare organizations can create a sustainable culture of well-being, empower nurses to prioritize their own health, and ultimately enhance the quality of care they provide.
Conclusion
The well-being of nurses is not merely a personal concern; it is a critical determinant of patient care quality and the overall strength of healthcare systems. In this context, the self care assessment tool for nurses emerges as an essential instrument for proactively addressing the unique stressors and demands faced by this vital professional group. By providing a structured means to evaluate self-care practices, identify areas of need, and monitor progress, these tools empower both individual nurses and healthcare organizations to prioritize well-being as a core component of professional nursing practice.
This article has highlighted the necessity of self care assessment tools for nurses, exploring the underlying concepts of self-care, the benefits of assessment, and the diverse types of tools available or adaptable for this purpose. From burnout and compassion fatigue measures to resilience and mindfulness scales, a range of instruments can provide valuable insights into the multifaceted nature of nurse well-being. Effective implementation, however, requires more than just tool selection. It demands a commitment to confidentiality, trust-building, integration with resources, and data-driven decision-making.
Looking ahead, further research and development are needed to refine and standardize self care assessment tools for nurses, ensuring their validity, reliability, and cultural relevance across diverse nursing populations and healthcare settings. Technological advancements may offer opportunities to integrate assessments into digital platforms, making them more accessible and user-friendly. Furthermore, future studies could explore the longitudinal impact of self-care assessment and intervention programs on nurse well-being, patient outcomes, and organizational performance.
Ultimately, the adoption and effective utilization of self care assessment tools for nurses represent a crucial step towards creating a healthcare environment that truly values and supports its caregivers. By prioritizing nurse well-being, organizations not only fulfill their ethical responsibility to their staff but also invest in a more resilient, compassionate, and effective nursing workforce, capable of providing the highest quality care to those they serve.
Author Contributions
Conceptualization, L.S., S.S., A.G., M.M., E.B., C.L. and L.C. (Adapted from original article); methodology, L.S., S.S., M.M., A.G. and L.C. (Adapted from original article); validation, L.S. and S.S. (Adapted from original article); formal analysis, L.S., S.S. and A.G. (Adapted from original article); investigation, L.S. and S.S. (Adapted from original article); data curation, L.S., S.S., M.M. and A.G. (Adapted from original article); writing—original draft preparation, AI; writing—review and editing, L.S., S.S., M.M., A.G., E.B., C.L. and L.C. (Adapted from original article), AI; visualization, AI; supervision, L.S., M.M. and L.C. (Adapted from original article); project administration, L.S., M.M. and L.C. (Adapted from original article). All authors have read and agreed to the published version of the manuscript. (Adapted from original article).
Institutional Review Board Statement
Not applicable. (Adapted from original article).
Informed Consent Statement
Not applicable. (Adapted from original article).
Conflicts of Interest
The authors declare no conflict of interest. (Adapted from original article).
Funding Statement
This research received no external funding. (Adapted from original article).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. (Adapted from original article).
References
(Keep references from original article and potentially add more relevant to assessment tools if found during writing. For now, retain original references as instructed).
[1] World Health Organization. Self-care interventions for health and well-being. Available online: https://www.who.int/news-room/fact-sheets/detail/self-care-interventions-for-health-and-well-being (accessed on 15 March 2023).
[2] Potter, P.A.; Perry, A.G. Fundamentals of Nursing; Mosby: St. Louis, MO, USA, 2005.
[3] Orem, D.E. Nursing: Concepts of Practice; Mosby: St. Louis, MO, USA, 1995.
[4] Geden, E.A. Revision of the concept self-care. Nurs. Sci. Q. 2009, 22, 155–160. [CrossRef] [PubMed]
[5] Barlow, J.; Wright, C.; Sheasby, J.; Turner, A.; Hainsworth, J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Couns. 2002, 48, 177–187. [CrossRef]
[6] Koloroutis, M. Relationship-Based Care: A Model for Transforming Practice; Creative Healthcare Management: Minneapolis, MN, USA, 2004.
[7] Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [CrossRef]
[8] Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review and meta-analysis. Brain Behav. Immun. 2020, 89, 531–542. [CrossRef]
[9] Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Rossi, A.; Molteni, M.; Balzarini, A.; Castelnuovo, G.; et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Brain Behav. Immun. 2020, 88, 189–190. [CrossRef]
[10] Lasalvia, A.; Amaddeo, F.; Grassi, L.; Lamonaca, D.; Bertelli, M.O.; Carrà, G.; Casanova, M.C.; Castelnuovo, G.; Cerveri, G.; De Lorenzo, R.; et al. Mental health conditions among healthcare workers during the COVID-19 pandemic and associated risk factors. A systematic review and meta-analysis. medRxiv 2020. [CrossRef]
[11] Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Nadkarni, S.; Malhotra, R.; Tam, W.W.L. A multinational, multicentre study on the psychological health of healthcare workers during the COVID-19 pandemic. Brain Behav. Immun. 2021, 91, 221–231. [CrossRef]
[12] Morgantini, L.A.; Naha, U.; Wang, H.; Wu, J.; Zhang, B.; Crivelli, D.E.; Punnett, L.; Pasha, J.A.; McAlonan, G.M.; Sharma, L.; et al. Factors contributing to healthcare professional burnout during COVID-19 pandemic: A systematic review and meta-analysis. medRxiv 2020. [CrossRef]
[13] Pfefferbaum, B.; North, C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [CrossRef] [PubMed]
[14] Greenberg, N.; Docherty, M.; Gnanapragasam, S.; Ford, C.; Hotopf, M.; Lawn, W.; Fear, N.T. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020, 368, m1211. [CrossRef] [PubMed]
[15] Sinclair, S.; McClement, S.; Raffin Bouchal, S.; Hack, T.F.; Hagen, N.A.; Downar, J.;的位置, C.L. What are helpful responses to healthcare provider compassion fatigue? A systematic review of qualitative studies. Palliat. Med. 2017, 31, 3–15. [CrossRef]
[16] Wentzel, D.; Brysiewicz, P. Compassion fatigue in nurses working in high-intensity environments. Int. Emerg. Nurs. 2016, 24, 44–49. [CrossRef]
[17] Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [CrossRef]
[18] Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Booth, A.; Donovan, T.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [CrossRef]
[19] Kmet, L.M.; Lee, R.C.; Cook, L.S. Standard quality assessment criteria for evaluating primary research papers from a variety of fields. 2004. Available online: https://www.ihe.ca/wp-content/uploads/2020/03/kmet-lee-cook-2004-standard-quality-assessment-criteria-for-evaluating-primary-research-papers-from-a-variety-of-fields.pdf (accessed on 15 March 2023).
[20] Andrews, J.; Ericsson, C.; Jansson, I.; Nordström, G. Nurses’ experiences of self-care and self-compassion in relation to compassionate care giving—A qualitative study. J. Clin. Nurs. 2020, 29, 2543–2554. [CrossRef] [PubMed]
[21] Blackburn, L.; Brown, J.; Rigg, K.; Blackburn, R.E. Evaluation of a resilience-based program to decrease burnout and secondary trauma in oncology staff. J. Oncol. Navig. Surviv. 2020, 11, 227–236.
[22] Craigie, M.; Osseiran-Moisson, R.; Hemsworth, D.; Wilson, C.; Bajorek, B.; Dawes, G.; Rees, C. Mindfulness-based program for nurses to reduce stress and improve well-being: A pilot study. Nurse Educ. Today 2016, 36, 81–89. [CrossRef]
[23] Delaney, L.J. Mindful self-compassion: An intervention to promote resilience and reduce burnout in nurses. Nurse Educ. Today 2018, 63, 177–182. [CrossRef]
[24] Duarte, J.; Pinto-Gouveia, J.; Cruz, B. Professional quality of life, empathy, and self-compassion of nurses—A correlational study. J. Nurs. Scholarsh. 2016, 48, 517–525. [CrossRef] [PubMed]
[25] Fourer, M.; Booth, J.; Daly, J.; Carey, M. Mindfulness based stress reduction for psychological distress in nurses and midwives: A systematic review and meta-analysis. JBI Database System. Rev. Implement. Rep. 2013, 11, 1–15.
[26] Hegney, D.; Rees, C.S.; Eley, R.; Osseiran-Moisson, R.;考考, L.; Baker, P.; Ross, J.; Watson, R.E.;талиа, T. The contribution of individual psychological resilience, negative affect and coping styles to nurses’ quality of life and turnover intention: A mixed methods study. J. Adv. Nurs. 2015, 71, 2359–2375. [CrossRef]
[27] Mahon, N.;干草, R.; Tyrell, F. Mindfulness meditation and self-compassion: A pilot study with nurses. Ir. J. Psychol. Med. 2017, 34, 293–299. [CrossRef]
[28] Mills, J.; Beanlands, H.; Ward-Griffin, C.;锶, S. Exploring relationships among self-care, self-compassion, and compassion in palliative care health professionals. J. Hosp. Palliat. Nurs. 2018, 20, 327–334. [CrossRef]
[29] Sallon, S.; выхода, T.; Band-Winterstein, T. Caring for the caregivers: Evaluation of a multimodal intervention to reduce stress and burnout and improve self-care and coping skills among hospital staff. Isr. J. Health Policy Res. 2015, 4, 32. [CrossRef]
[30] Slatyer, S.; Osseiran-Moisson, R.; Pearse, J.;
