Mental health is a critical component of overall well-being, yet depression and anxiety disorders remain significantly underdiagnosed and undertreated, particularly within primary care settings. Recognizing this gap, healthcare providers and organizations are increasingly emphasizing the importance of routine screening for these conditions. This article explores the crucial role of screening tools for depression and anxiety in primary care, drawing upon evidence-based practices and quality improvement initiatives to highlight their effectiveness and implementation strategies.
The Imperative for Mental Health Screening in Primary Care
Depression and anxiety are among the most prevalent mental health disorders worldwide. In the United States alone, millions of adults experience major depressive episodes and anxiety disorders annually, leading to substantial personal suffering, reduced productivity, and increased healthcare costs. These conditions are often comorbid with chronic physical illnesses, further complicating patient care and outcomes.
Primary care settings serve as the frontline of healthcare for many individuals, making them an ideal point of contact for early identification and intervention for mental health conditions. The U.S. Preventive Services Task Force (USPSTF) recommends universal depression screening for adults in primary care, advocating for integrated systems that combine screening with evidence-based treatment protocols. Similar recommendations are emerging for anxiety screening to address the full spectrum of common mental health challenges.
Early detection and treatment of depression and anxiety in primary care offer numerous benefits:
- Improved Patient Outcomes: Timely intervention can alleviate symptoms, improve quality of life, and reduce the long-term impact of these disorders.
- Reduced Healthcare Costs: Addressing mental health conditions proactively can decrease the need for more intensive and costly interventions later on.
- Enhanced Productivity: Effective treatment can help individuals return to work and maintain fulfilling lives.
- Better Management of Comorbidities: Recognizing and treating depression and anxiety can improve the management of co-existing physical health conditions.
Validated Screening Tools for Depression and Anxiety
To facilitate efficient and accurate screening in busy primary care settings, several validated tools are available for depression and anxiety. These tools are designed to be brief, easy to administer, and reliable in identifying individuals who may require further assessment and treatment.
Depression Screening Tools
The Patient Health Questionnaire (PHQ) family of tools are widely recognized and utilized for depression screening in primary care.
- PHQ-2: This ultra-brief two-item questionnaire screens for the core symptoms of depression: depressed mood and anhedonia (loss of interest or pleasure). A score of 3 or higher is considered a positive screen, indicating the need for further evaluation.
- PHQ-9: A more comprehensive 9-item questionnaire, the PHQ-9 aligns with the DSM-5 criteria for major depressive disorder. It assesses the severity of depression symptoms and can be used to monitor treatment progress. Scores correspond to different levels of depression severity, from mild to severe.
Anxiety Screening Tools
For anxiety disorders, the Generalized Anxiety Disorder 7-item scale (GAD-7) is a commonly used and effective screening instrument in primary care.
- GAD-7: This 7-item questionnaire assesses the frequency and severity of generalized anxiety symptoms over the past two weeks. It is quick to administer and has demonstrated good sensitivity and specificity for detecting generalized anxiety disorder, as well as other anxiety disorders like panic disorder and social anxiety disorder. Scores on the GAD-7 also correlate with levels of anxiety severity.
While PHQ tools are primarily for depression and GAD-7 for generalized anxiety, it’s important to note that anxiety and depression often co-occur. Some combined screening tools or approaches may be considered to efficiently address both.
Integrating Screening into Primary Care Workflow: Measurement-Based Care
Effective implementation of screening tools requires a systematic approach that seamlessly integrates into the existing primary care workflow. Measurement-Based Care (MBC) offers a structured framework for this integration. MBC involves:
- Routine Screening: Using validated tools like PHQ-2, PHQ-9, and GAD-7 to screen all adult patients for depression and anxiety.
- Standardized Assessment: Utilizing the results of screening tools, along with clinical interviews, to accurately diagnose mental health conditions.
- Treatment Planning: Developing personalized treatment plans based on evidence-based guidelines and patient preferences. This might include pharmacological interventions, psychotherapy, lifestyle modifications, or a combination of approaches.
- Symptom Monitoring: Regularly tracking patient symptoms using the same screening tools or other standardized measures to assess treatment response and make adjustments as needed.
- Referral Systems: Establishing clear pathways for referral to mental health specialists when necessary.
Technology plays a crucial role in facilitating MBC. Electronic Health Records (EHRs) can be integrated with screening tools to automate administration, scoring, and data capture. Clinical Decision Support (CDS) systems within EHRs can provide prompts and guidance to primary care providers based on screening results and patient data, ensuring consistent and evidence-based care.
Example of Successful Implementation: The VitalSign6 Program
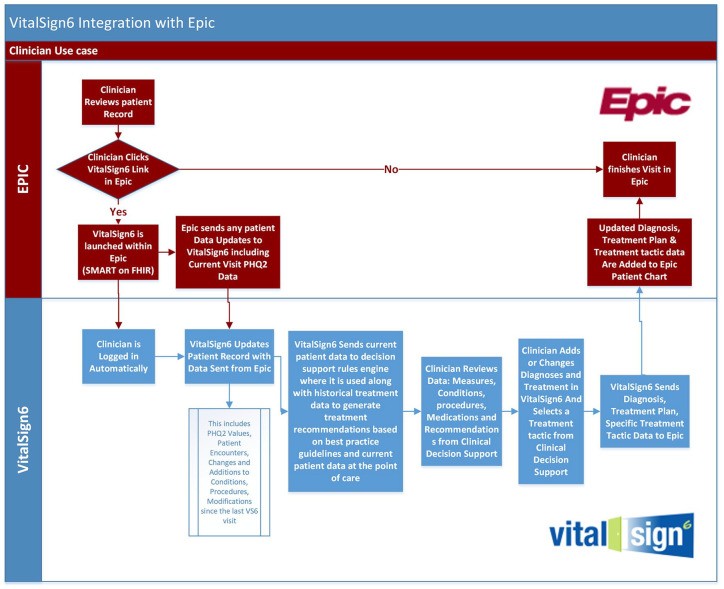
The VitalSign6 program, as highlighted in the original article, provides a compelling example of successful MBC implementation in primary care. This program utilized a web-based application integrated with the EHR to streamline depression screening and management.
Key features of VitalSign6 included:
- EHR Integration: Seamless integration with the EHR system using application programming interfaces (APIs) for real-time data exchange.
- Digital Screening Tools: Administration of PHQ-2 and PHQ-9 questionnaires on tablets within the clinic workflow.
- Clinical Decision Support: Algorithm-based decision support tools to guide diagnosis, treatment selection, and follow-up.
- Symptom Tracking: Tools for monitoring symptom severity and treatment response over time.
The implementation of VitalSign6 in a primary care clinic resulted in significant improvements in depression screening rates and a notable decrease in self-reported depression scores among patients receiving treatment. While the program primarily focused on depression, the principles and technological infrastructure could be adapted to include anxiety screening and management using tools like GAD-7.
Addressing Challenges and Optimizing Implementation
Despite the clear benefits of screening tools and MBC, successful implementation in primary care can face challenges. These may include:
- Workflow Disruption: Integrating new screening processes into already busy clinics can be perceived as disruptive to workflow.
- Time Constraints: Primary care providers often face time limitations, and incorporating mental health screening needs to be efficient.
- Technical Issues: EHR integration and technical glitches can hinder smooth implementation.
- Provider Training and Buy-in: Adequate training and engagement of primary care providers and staff are essential for successful adoption.
- Follow-up and Treatment Capacity: Effective screening must be linked to adequate follow-up and treatment resources, either within the primary care setting or through accessible referral pathways.
To overcome these challenges, strategies such as:
- Streamlining Workflow: Designing efficient screening processes that minimize disruption and time burden.
- Leveraging Technology: Utilizing EHR integration and CDS tools to automate tasks and provide decision support.
- Providing Training and Support: Offering comprehensive training to primary care teams on screening tools, MBC principles, and available resources.
- Building Integrated Care Models: Developing collaborative care models that integrate mental health professionals within primary care settings.
- Ensuring Follow-up and Referral Pathways: Establishing clear and accessible pathways for mental health treatment and specialist referrals.
Conclusion: Enhancing Mental Healthcare Through Primary Care Screening
Screening tools for depression and anxiety are invaluable assets in primary care settings. Their systematic implementation, within a framework like Measurement-Based Care, can significantly improve the early identification and management of these common mental health disorders. By prioritizing mental health screening, primary care practices can enhance patient outcomes, reduce healthcare burdens, and contribute to a more integrated and holistic approach to healthcare. Continued efforts to refine implementation strategies, leverage technology, and build integrated care models will be crucial to fully realize the potential of primary care in addressing the mental health needs of the population.
References