Introduction
In the evolving landscape of healthcare, enhancing the quality of care while managing costs is a paramount objective. In the United States, healthcare reform is driven by the “triple aim” of improving patient care, enhancing population health, and reducing healthcare expenditures. A significant area for improvement lies in reducing unnecessary hospitalizations and readmissions, particularly for vulnerable long-term care (LTC) residents. These transfers can lead to hospital-acquired complications, increased morbidity and mortality, and substantial financial burdens. Studies suggest that a considerable portion of these hospitalizations are preventable, offering potential savings in Medicare and Medicaid spending. This is where targeted interventions like the INTERACT (Interventions to Reduce Acute Care Transfers) program become invaluable. This review focuses on the Interact Quality Improvement Tool For Review Of Acute Care Transfers, a key component designed to empower nursing homes to systematically analyze and reduce avoidable hospital transfers, aligning with national healthcare quality and cost-efficiency goals.
Understanding the Need for Quality Improvement in Acute Care Transfers
The healthcare sector, especially geriatric care, stands at a crucial juncture. Healthcare professionals in LTC facilities are uniquely positioned to lead improvements in care delivery models and contribute to cost savings. The Centers for Medicare and Medicaid Services (CMS) recognizes this potential, funding initiatives aimed at enhancing quality and minimizing unnecessary hospitalizations in nursing homes. Several interventions focusing on care transitions have emerged as effective strategies. These include guidelines from the American Medical Directors Association and models utilizing advanced practice nurses to bridge hospital and LTC settings. Projects like Re-Engineered Discharge (RED) adapted for nursing homes and palliative care consultation services have also shown promise.
Among these interventions, INTERACT stands out as a comprehensive quality improvement program widely adopted across the United States and internationally. Active implementation of INTERACT has been linked to significant reductions in hospitalizations – up to 24% in some studies. Such reductions translate to considerable Medicare savings for participating nursing homes. However, like any quality improvement initiative, INTERACT’s success hinges on the commitment of an interdisciplinary leadership team, including medical directors, directors of nursing, administrators, and primary care clinicians. This review aims to provide an overview of the INTERACT program, particularly emphasizing its quality improvement tools, to encourage its adoption and champion its principles in reducing unnecessary acute care transfers and readmissions.
The Development and Evolution of INTERACT
The INTERACT program originated from a CMS-funded project by the Georgia Medical Care Foundation, aimed at enhancing care quality within Georgia’s Medicare Quality Improvement Organization. Through detailed analysis of hospitalization patterns in Georgia nursing homes and expert panel reviews, a toolkit was developed and pilot-tested in facilities with high hospitalization rates. Initial results were promising, showing a 50% reduction in hospitalization rates and a 36% decrease in avoidable hospitalizations in pilot sites.
With further support from The Commonwealth Fund, the INTERACT toolkit underwent refinement through expert reviews and feedback from nursing home providers. A collaborative quality improvement project involving 30 nursing homes across three states further validated the program’s effectiveness, demonstrating a 17% reduction in all-cause hospitalizations, with engaged facilities achieving a 24% reduction. While these early studies were not randomized controlled trials, they provided strong evidence of INTERACT’s feasibility and impact in reducing hospitalizations.
Continued refinement, leading to INTERACT Version 3.0, involved ongoing expert input and user feedback. These updated tools are freely accessible at http://interact.fau.edu. Currently, INTERACT Version 3.0 is undergoing rigorous evaluation in a large-scale randomized controlled quality improvement project supported by the National Institutes of Health, with results expected to further solidify its evidence base.
Core Components of the INTERACT Program: A Focus on Quality Improvement
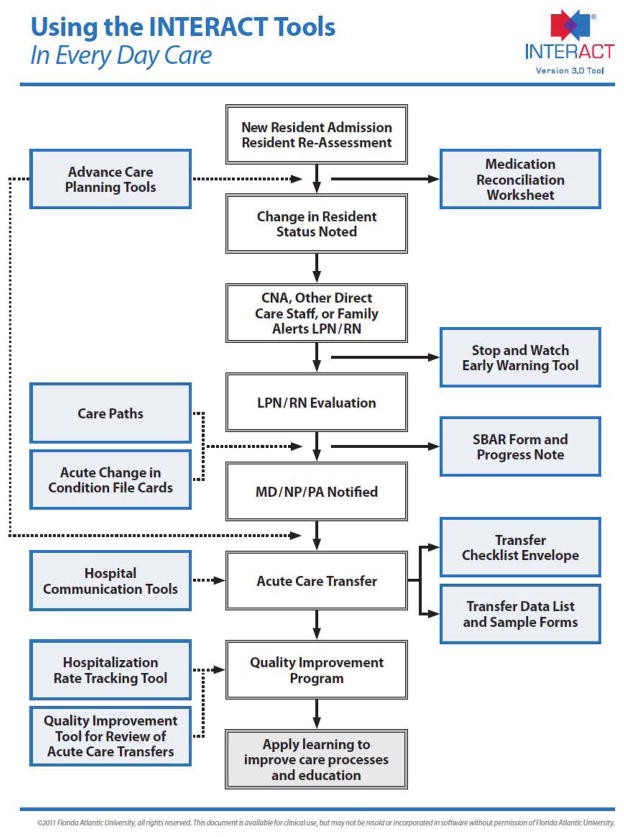
The INTERACT program is structured around five fundamental strategies, visualized in Figure 1, designed to be integrated into the daily routines of nursing home care. Moving beyond a simple toolkit, INTERACT is now recognized as a comprehensive quality improvement program focused on enhancing the management of acute changes in resident conditions. The primary goal is to safely manage conditions within the nursing home setting, avoiding unnecessary hospitalizations.
Figure 1. Overview of the INTERACT Program in Every Day Care.
This figure illustrates the cyclical nature of INTERACT, embedding quality improvement into every aspect of nursing home care, from admission to discharge and beyond. The key strategies are:
- Quality Improvement Principles: This cornerstone involves establishing a team-based approach led by a champion, securing strong leadership support, implementing measurement and tracking of outcomes, and crucially, conducting root cause analyses of hospitalizations to drive continuous learning and improvement. This is where the INTERACT Quality Improvement Tool plays a pivotal role.
- Early Identification and Evaluation of Changes in Condition: Proactive detection of subtle changes in a resident’s health status before they escalate is critical.
- Management of Common Changes in Condition: Providing protocols and resources to manage conditions within the nursing home when it is safe and feasible to do so.
- Improved Advance Care Planning: Ensuring residents’ wishes are known and honored, especially regarding hospitalization preferences, and utilizing palliative or hospice care when appropriate.
- Improved Communication and Documentation: Streamlining communication within the nursing home team, with families, and with hospitals to ensure seamless care transitions.
INTERACT Quality Improvement Tools: Analyzing Acute Care Transfers
A core element of effective quality improvement is the ability to track, analyze, and learn from data. INTERACT provides specific tools to facilitate this, particularly focusing on the review of acute care transfers. The INTERACT Quality Improvement Tool is specifically designed for performing root cause analyses of individual hospital transfers. This tool enables nursing home staff to systematically investigate each transfer to understand the factors that contributed to it and identify potential areas for improvement.
Complementing this individual review tool is the Quality Improvement Summary Worksheet. This worksheet guides users in aggregating data from individual transfer reviews to identify trends and patterns. By summarizing the findings from multiple root cause analyses, facilities can pinpoint common issues, such as prevalent changes in condition leading to transfers or recurring communication breakdowns. This aggregated data is crucial for targeting educational efforts and refining care processes to prevent future unnecessary transfers.
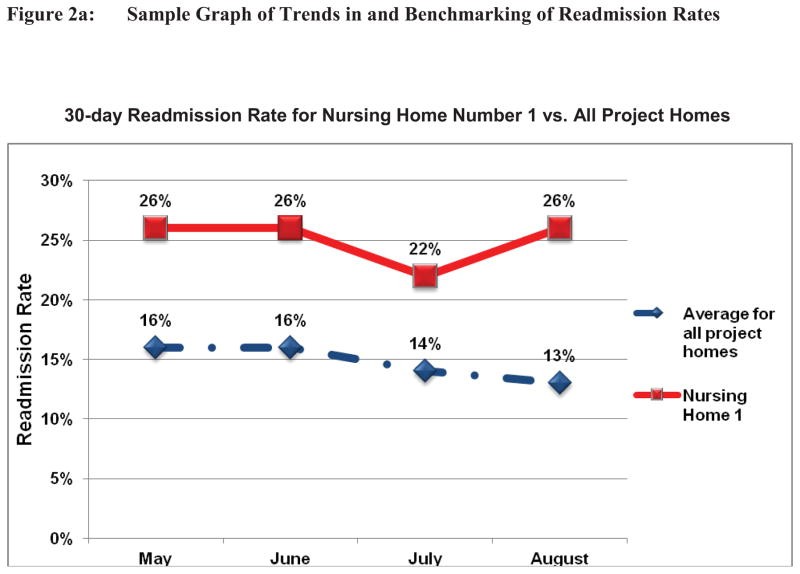
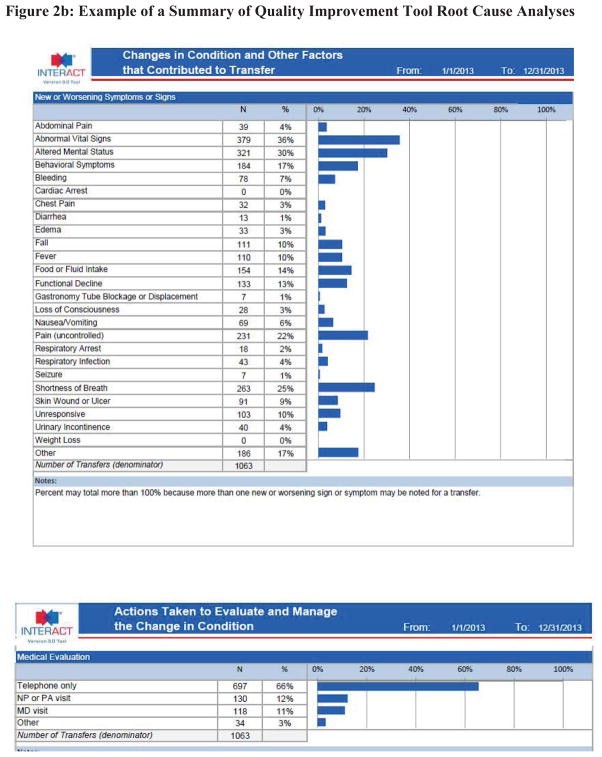
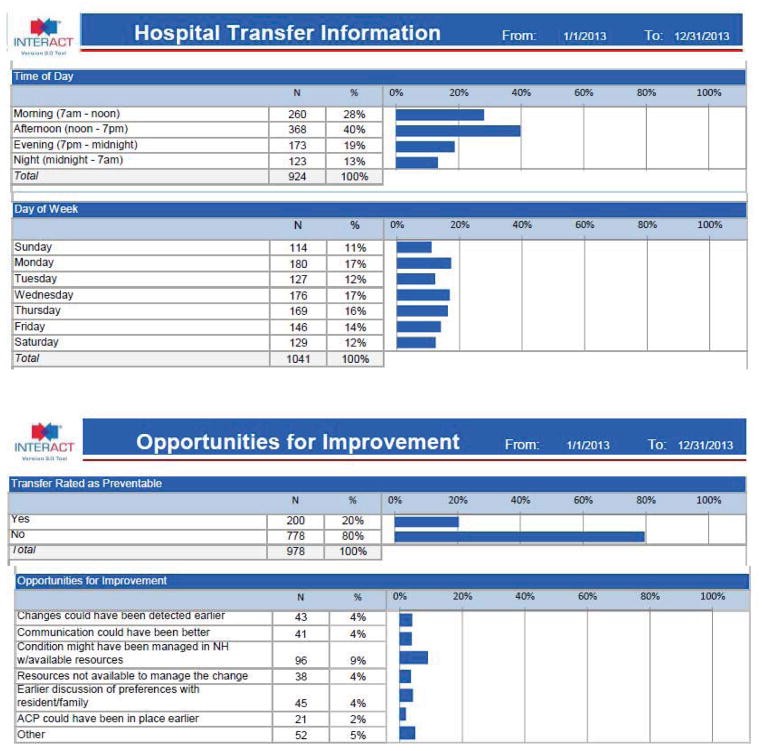
The output from these quality improvement tools can be visualized using “quality dashboards,” as exemplified in Figure 2. These dashboards provide a clear and concise overview of key performance indicators, such as 30-day readmission rates and the summarized data from root cause analyses.
Figure 2. Example of an INTERACT Quality Improvement Dashboard.
Figure 2a demonstrates how 30-day readmission rates can be tracked over time and benchmarked against other facilities. Figure 2b illustrates the summary of root cause analysis data, highlighting common changes in condition associated with transfers, shift timings, and weekend occurrences, as well as the proportion of potentially preventable transfers. This visual representation of data empowers nursing homes to monitor their progress, identify areas needing attention, and demonstrate the impact of their quality improvement efforts.
Complementary INTERACT Tools for Enhanced Care and Communication
While the Quality Improvement Tool is central to reviewing transfers, other INTERACT tools support the broader goal of reducing unnecessary hospitalizations by improving early detection, communication, and decision-making.
The “STOP and WATCH” Tool serves as an early warning system, designed for certified nursing assistants (CNAs) and other direct care staff, including non-clinical staff and families. It uses simple language to identify subtle, early changes in a resident’s condition, prompting timely assessment by licensed nurses.
The “SBAR Communication Form and Progress Note” provides a structured framework for nurses to evaluate changes in condition and communicate effectively with primary care clinicians. Based on the Situation, Background, Assessment, Recommendation (SBAR) method, this tool ensures nurses provide comprehensive and relevant information, facilitating informed decisions and reducing unnecessary emergency room transfers due to inadequate communication.
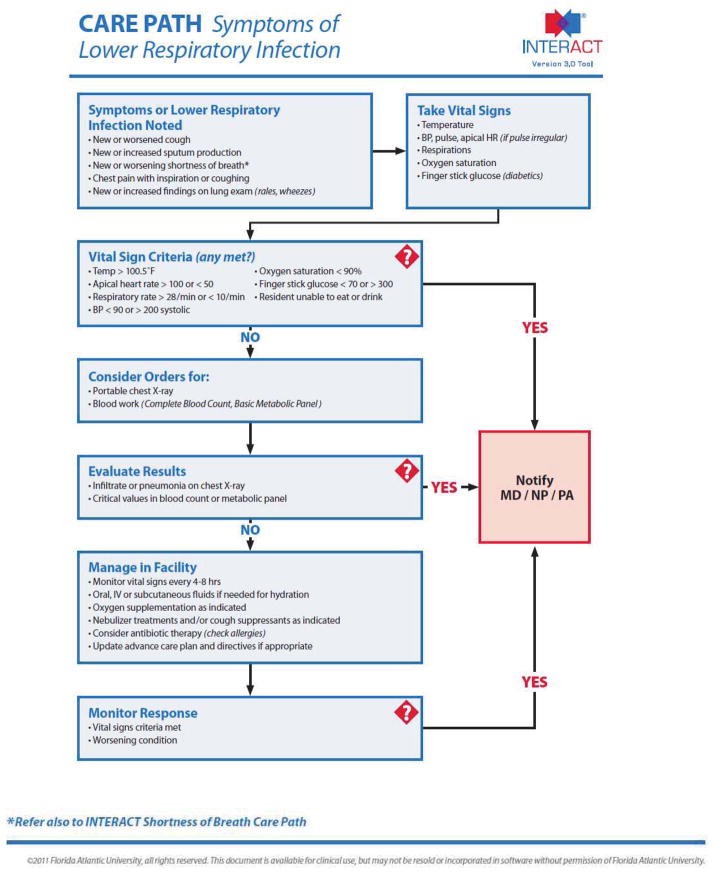
Decision Support Tools, including Change in Condition File Cards and Care Paths, offer guidance on evaluating and managing specific changes in condition. These tools, while based on expert consensus and clinical guidelines, are designed to support clinical judgment, not replace it. They provide a systematic approach to common symptoms and conditions, promoting consistent responses and clear communication criteria. Figure 3 illustrates an example of an INTERACT Care Path.
Figure 3. Example of an INTERACT Care Path.
Advance Care Planning Tools facilitate discussions with residents and families about their care preferences, particularly regarding hospitalization. These tools emphasize that advance care planning is a team effort and should be revisited at admission, regularly, and during changes in condition.
Hospital Communication Tools streamline information exchange during transfers, including checklists for essential transfer documents and forms to document critical patient data. The “Nursing Home to Hospital Transfer Form” and “Hospital to Post-Acute Care Transfer Form” are designed to ensure hospitals receive the necessary information for informed decision-making and that nursing homes receive crucial post-hospitalization details for seamless care.
Keys to Successful INTERACT Implementation and Overcoming Barriers
Successful implementation of INTERACT, and effective utilization of its quality improvement tools, depends on several key factors, summarized in Table 1.
Table 1.
Keys to Successful INTERACT Implementation
| Examples of Successful Implementation Strategies | Examples of Common Barriers to Implementation and How They Are Overcome |
|---|---|
| Executive Leadership Support for the INTERACT Quality Improvement Program(Executive Leaders include Executive Directors, Administrators, Directors of Nursing, Corporate Leaders if applicable, Medical Directors, Clinical Pharmacists) | Articulates vision and commitment regarding the purpose and goals for using INTERACT to the entire staff.Demonstrates commitment by: – Allocating sufficient time for staff training – Attending relevant training sessions – Promoting formation of multidisciplinary team to plan/deliver/and sustain inclusion of INTERACT into standards of care for facility – Participating in review and discussion of data including acute care transfer rates and summary of Quality Improvement Review Tools Uses data to motivate staff internally and to articulate the unique value that their facility brings to cross continuum partners in efforts to reduce unnecessary acute care transfers.Initiates contact with local hospitals to establish relationship and promote collaboration |
| Engagement of Direct Care Staff by INTERACT Champion(s)(Selection of a Champion(s) is one of the most important decisions to be made. Successful implementation depends on the right person(s) in this role.) | Criteria for the role of INTERACT Champion(s):Is able to motivate staff to attend training sessions and to try new toolsHas experience providing training and education.Has formal or informal authority to drive/influence change in staff behavior and practice.Provides training and directs process improvement using NON PUNITIVE approach.Agrees or volunteers to be champion.Activities of effective champions: – Visible on the units daily – Communicates enthusiasm for the program – Reminds staff to use tools – Makes tools visible and accessible for everyday use – Seeks and responds to staff input on how to use tools most effectively – Collaborates with key staff members on the evening/night/weekend shifts to promote consistent use of the INTERACT program on all days/shifts |
| Facility Culture Dedicated to Quality Improvement | The INTERACT program is an integral component of the facility’s quality improvement activities and QAPI programINTERACT training and implementation are delivered using a non-punitive approach.When avoidable hospitalizations are identified, a spirit of inquiry by the multidisciplinary team seeks improvement, not blame |
Executive leadership support is crucial for allocating resources and championing the program. Engaged INTERACT champions are essential for motivating staff and driving implementation at the unit level. Finally, a facility-wide culture dedicated to quality improvement, where data is used for learning and improvement rather than blame, is fundamental to sustained success. Addressing common barriers, such as resistance to change, time constraints, and the perception of external pressures to transfer, requires proactive strategies and a commitment to embedding INTERACT principles into routine practice.
INTERACT’s Role in Quality Assurance and Performance Improvement (QAPI)
The Affordable Care Act mandates Quality Assurance Performance Improvement (QAPI) programs in nursing homes. INTERACT provides a robust framework to meet these requirements, particularly in reducing hospital readmissions, a key focus for both QAPI and Accountable Care Organizations (ACOs). Many nursing homes lack the infrastructure for comprehensive QAPI plans, and INTERACT offers a structured approach to develop and implement these plans, enhancing their attractiveness as partners to ACOs.
While reducing hospital transfers is a primary goal, INTERACT’s comprehensive approach aligns with the five elements of QAPI outlined by CMS, as shown in Table 2. By implementing INTERACT fully, facilities can demonstrate a commitment to systematic quality improvement, addressing multiple care processes across the organization.
Table 2.
QAPI Elements Related to INTERACT Program Processes
| QAPI Element | INTERACT Processes |
|---|---|
| Design and Scope | Staff from all departments participate in INTERACT trainingStaff from all departments and families are invited to complete “Stop and Watch” tool if they detect a change in conditionResidents who are hospitalized are discussed at team meetings or morning report with all department heads and other staff present. |
| Leadership and Governance | Letters of invitation to facility and corporate leadership and other materials stress the critical role of leadership engagement in INTERACT implementation. Training modules describe the vital role of leadership in providing resources for INTERACT implementation and the need for an ongoing dialogue between leadership and direct care staff.Reports from the QI review tool may be shared with leadership and the Board so that they can determine next action steps.Board members are actively engaged with direct care staff and families, are visible on the units and can articulate QAPI principles to families and staff. |
| Feedback, Data systems and Monitoring | SBAR tool enhances communication, feedback and monitoring between nurses and primary care providers.Stop and Watch tool enhances communication among CNAs, other staff, family members and nurses. Nurses provide feedback to direct care staff about their completion rates of the Stop and Watch tool, as well as the quality of the information.The QI review tool generates data and reports that are shared with direct care staff. Changes in attitudes and behaviors with respect to early identification of change in condition are monitored by supervisors and leadership, and an open dialogue is encouraged.Staff may use the transfer log and the list of people with a change in condition who are not transferred to review the decisions to transfer or not to transfer and make appropriate practice changes based on data. Input from direct care staff is encouraged, valued and accepted in a non-punitive atmosphere. |
| Performance Improvement Projects (PIPs) | Decision support tools such as the care paths can be implemented and tested in a PIP and modified to meet the specific needs of an individual facility.Data from the QI review tools may lead to prioritizing decisions about areas of concern that may merit PIPs. For example, if transfers are occurring due to bleeding and it is noted that INR values are often out of range, a PIP with respect to lab monitoring might be initiated. |
| Systematic Analysis and Systemic Action | The reports generated from QI review tools, as well as reports that could be shared based on completion of SBAR or Stop and Watch data provide patterns and help to identify fundamental, systemic issues throughout the facility such as failures in communication, weak teamwork, inadequate documentation, delays in relaying critical information across departments, etc.Networking with cross-continuum teams and hospital partners supports enhanced and seamless care across transitions and provider types that consider the nursing home part of the larger health care system.Principles in the Advance Care Planning tools support patient and family engagement, person-centered care and a focus on patient self-determination of their goals of care. Consistent implementation of those tools represents systemic action throughout the facility. |
The INTERACT Quality Improvement Tool directly supports QAPI by providing a mechanism for data-driven performance improvement. The systematic analysis of transfers, identification of trends, and implementation of targeted interventions based on QI tool data are all core components of an effective QAPI program. By integrating INTERACT comprehensively, nursing homes can move beyond disparate initiatives and create a truly system-based approach to quality improvement.
Conclusion
The INTERACT program, with its suite of tools, particularly the INTERACT quality improvement tool for review of acute care transfers, offers a practical and effective approach to reducing unnecessary hospitalizations in nursing homes. By focusing on early identification, structured communication, decision support, and advance care planning, and by emphasizing continuous quality improvement, INTERACT empowers nursing homes to enhance resident care, reduce costs, and meet evolving regulatory requirements like QAPI. Familiarity and active support from medical directors, primary care clinicians, and nursing home leadership are crucial for the successful and sustainable implementation of INTERACT, ensuring its benefits are fully realized in improving the lives of nursing home residents and the efficiency of the healthcare system.
Acknowledgments
The development and testing of the INTERACT program has been supported by the National Institutes of Health (1R01NR012936), the Centers for Medicare and Medicaid Services, The Commonwealth Fund, The Retirement Research Foundation, the Patient Centered Outcomes Research Institute, Medline Industries, and Westcom, Inc.
Footnotes
Publisher’s Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.

