This article explores the importance of point of care (POC) leadership for registered nurses in implementing evidence-based practices (EBPs) and reviews two leadership measurement tools: the Implementation Leadership Scale (ILS) and the iLEAD.
 alt text: A group of nurses collaborating around a patient's chart, demonstrating point of care leadership in action.
alt text: A group of nurses collaborating around a patient's chart, demonstrating point of care leadership in action.
The Importance of Point of Care Leadership in Nursing
Effective leadership at the point of care is crucial for successful EBP implementation in nursing. While general leadership principles are important, implementation leadership (IL) focuses on specific behaviors that facilitate the uptake of EBPs. These behaviors include proactive planning, knowledgeable decision-making, supportive mentorship, and perseverant efforts in overcoming implementation barriers. POC nurse leaders, including nurse managers, advanced practice nurses, educators, and champions, play key roles in fostering a positive implementation climate.
Implementation Leadership Measurement Tools: ILS and iLEAD
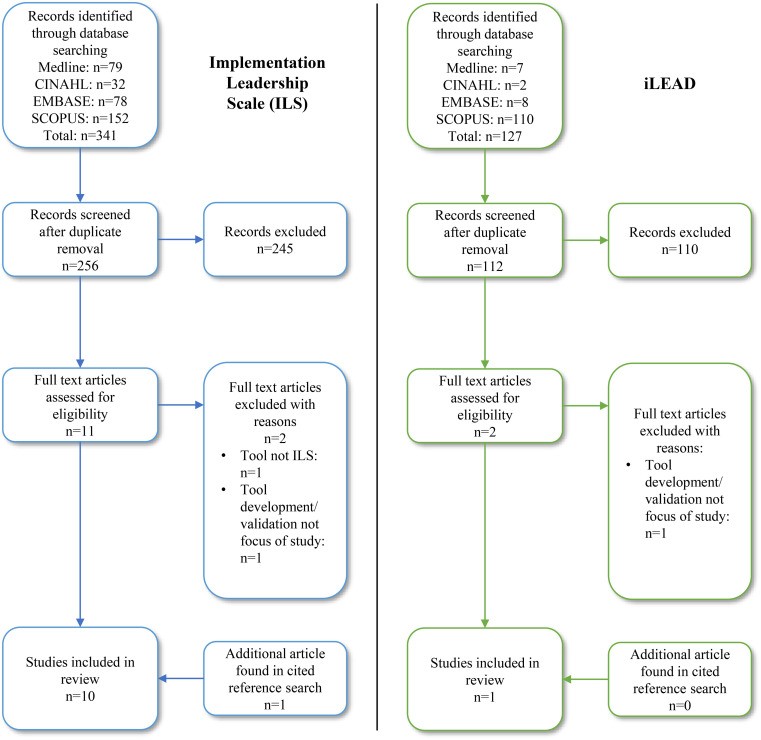
Two tools designed to measure IL are the Implementation Leadership Scale (ILS) and the iLEAD.
Implementation Leadership Scale (ILS)
The ILS assesses IL from the perspectives of both leaders (ILS-Leader) and staff (ILS-Staff). It comprises 12 items across four subscales: Proactive Leadership, Knowledgeable Leadership, Supportive Leadership, and Perseverant Leadership. Each item uses a 5-point Likert scale (0-4), generating subscale and total scores. The ILS has been translated and validated in multiple languages, including Chinese and Greek. A shortened, adapted version (ILS-Adapted) also exists.
iLEAD
The iLEAD measures employee perceptions of leader behaviors related to EBP implementation. Based on the Full Range Leadership Model (FRLM), it includes 16 items categorized into Active and Passive IL. The Active IL factor further divides into four subscales: Exemplary Behaviors, Individualized Consideration, Intellectual Stimulation, and Contingent Reward. Responses are recorded on a 5-point Likert scale (1-5), with mean scores calculated for each factor and subscale.
Critical Appraisal of the ILS and iLEAD
A systematic review of studies evaluating the ILS and iLEAD revealed strengths and limitations of both tools.
Strengths
- ILS: Demonstrated strong psychometric properties in various healthcare settings, including nursing. Available in multiple languages and freely accessible online. Mapped to the Ottawa Model of Implementation Leadership (O-MILe), strengthening its theoretical foundation.
- iLEAD: Based on the well-established FRLM, providing a framework for understanding leadership behaviors. Showed good psychometric properties in a healthcare setting. Distinguishes between active and passive leadership behaviors.
Limitations
- Both Tools: Limited reporting on item development and content validation processes raises concerns about the tools’ foundational rigor. Further research is needed to confirm content validity with diverse nursing experts.
- ILS: Requires further validation specifically within the context of diverse nursing leadership roles at the POC, including shared leadership models and the contributions of champions.
- iLEAD: Lacks specific validation within nursing contexts. Its foundation on a general leadership model, rather than a specific IL model, may limit its ability to capture nuances of implementation leadership in nursing.
Implications for Registered Nurses
Understanding and utilizing effective IL behaviors are crucial for registered nurses involved in EBP implementation. The ILS and iLEAD offer potential for assessing and developing IL competencies in nursing. However, selecting the appropriate tool requires careful consideration of its strengths, limitations, and contextual relevance. Future research should focus on strengthening the theoretical underpinnings and content validity of both tools within diverse nursing settings. Furthermore, exploring the feasibility of these tools in real-world nursing practice is essential. This includes considerations of time constraints, ease of administration, and interpretability of results.
Future Directions
Future research should prioritize:
- Rigorous content validation: Engage diverse nursing experts in evaluating the relevance and comprehensiveness of items in both the ILS and iLEAD.
- Context-specific validation: Conduct studies to validate the tools in settings reflecting the diverse and often shared leadership structures within nursing units.
- Feasibility studies: Assess the practicality of using these tools in real-world nursing settings, considering factors such as time constraints and ease of interpretation.
- Development of nursing-specific IL tools: Explore the need for developing tools specifically tailored to the unique challenges and opportunities of IL within nursing.
By addressing these areas, we can enhance our understanding of IL in nursing and develop effective strategies for fostering a leadership environment that promotes successful EBP implementation and ultimately improves patient care.
